Short-Stem Total Hip Arthroplasty: The Future of Hip Replacement Surgery
Short-Stem Total Hip Arthroplasty: Benefits, Recovery & Top Implants Explained

When hip pain becomes unbearable and everyday activities feel like an uphill battle, a total hip replacement can be life-changing. But not all hip replacements are the same — and in recent years, short-stem total hip arthroplasty has emerged as a groundbreaking alternative to traditional hip implants.
Whether you're an active individual looking to preserve mobility or a younger patient seeking a long-lasting solution, short-stem implants offer faster recovery, improved biomechanics, and better bone preservation — making them an increasingly popular choice among both patients and surgeons.
But what exactly makes a short-stem hip replacement different from the traditional approach? And which short-stem implant is right for you?
In this ultimate guide, we’ll dive into everything you need to know — from the science behind short-stem technology to side-by-side comparisons of leading implants — helping you make an informed, confident decision about your hip health.
Let’s explore why short-stem total hip arthroplasty is reshaping the future of hip replacements — and how it could transform your quality of life.
1. Introduction
Total hip arthroplasty (THA), commonly known as hip replacement surgery, has been a transformative procedure in orthopedic medicine, offering relief and improved mobility to countless individuals suffering from hip joint disorders. In recent years, the advent of short-stem implants has introduced a new dimension to hip replacement options, aiming to preserve more bone and potentially offer better outcomes for certain patient populations. This comprehensive guide delves into the intricacies of short-stem total hip arthroplasty, exploring its benefits, surgical techniques, patient selection criteria, and more.
2. Anatomy of the Hip Joint
The hip joint is a ball-and-socket synovial joint, comprising the femoral head (the ball) and the acetabulum of the pelvis (the socket). This joint structure allows for a wide range of motion, enabling activities such as walking, running, and sitting. The joint's stability is maintained by a combination of ligaments, tendons, and muscles, all working in harmony to facilitate movement and bear the body's weight.
3. Understanding Hip Arthritis
Arthritis, particularly osteoarthritis, is a leading cause of hip pain and disability. This degenerative condition results from the gradual wear and tear of the cartilage that cushions the hip joint, leading to pain, stiffness, and reduced mobility. Other forms of arthritis, such as rheumatoid arthritis, can also affect the hip joint, causing inflammation and joint damage.
4. Evolution of Hip Replacement Surgery
The journey of hip replacement surgery began in the early 20th century, with significant advancements over the decades. Traditional hip replacements involved longer stems inserted deep into the femur for stability. While effective, these designs could lead to complications such as bone loss and stress shielding. The development of short-stem implants emerged as a solution to these challenges, offering a bone-preserving alternative that aligns with the body's natural biomechanics.
5. What is Short-Stem Total Hip Arthroplasty?
Short-stem total hip arthroplasty involves the use of a femoral implant with a reduced stem length compared to traditional designs. These implants are designed to fit into the proximal femur, preserving more of the patient's natural bone and potentially offering a more physiological load distribution. This approach aims to reduce the risk of complications associated with longer stems and improve patient outcomes.
6. Indications for Short-Stem Hip Replacement
Short-stem hip replacements are particularly suitable for younger, active patients with good bone quality. They are also considered for patients requiring revision surgeries where bone preservation is crucial. However, patient selection is critical, and factors such as bone density, anatomy, and overall health play a significant role in determining the appropriateness of this implant type.
7. Advantages of Short-Stem Implants
The benefits of short-stem implants include:
- Bone Preservation: By conserving more of the femoral bone, these implants facilitate easier future revisions if necessary.
- Improved Biomechanics: Short-stem designs aim to mimic the natural biomechanics of the hip, potentially leading to better functional outcomes.
- Reduced Stress Shielding: The design promotes a more natural load distribution, minimizing the risk of bone resorption associated with stress shielding.
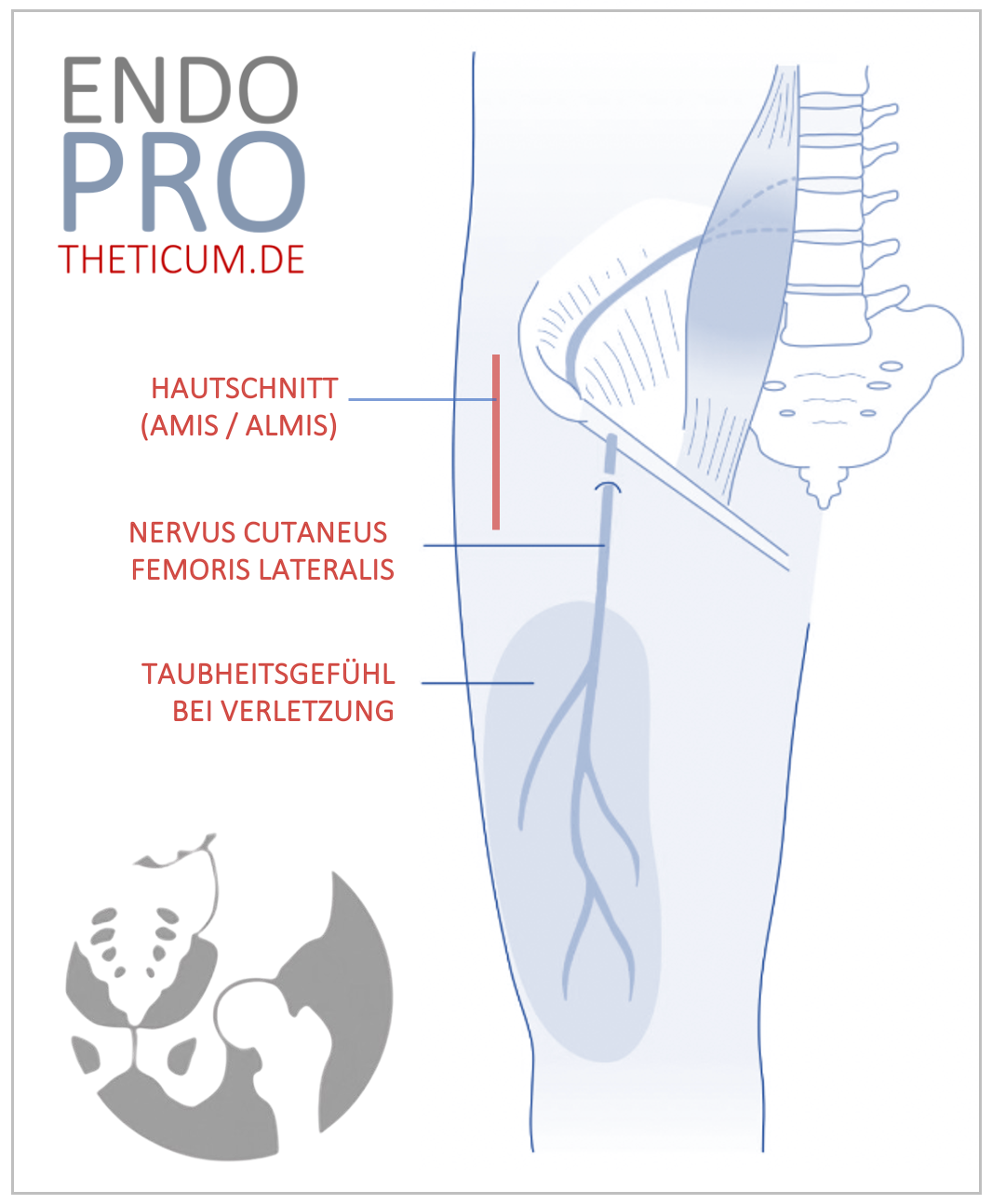
8. Surgical Techniques in Short-Stem Hip Arthroplasty
The surgical approach for short-stem hip arthroplasty requires meticulous planning and execution. Surgeons must be familiar with the specific implant system and its instrumentation. The procedure involves precise bone preparation to ensure optimal implant fit and stability. Minimally invasive techniques may be employed to reduce soft tissue damage and promote faster recovery.
9. Postoperative Rehabilitation and Recovery
Rehabilitation is a critical component of successful hip replacement surgery. Patients typically begin weight-bearing activities shortly after surgery, with a structured physiotherapy program to restore strength, flexibility, and function. Adherence to rehabilitation protocols is essential to achieve the best possible outcomes.
10. Potential Complications and Their Management
While short-stem hip arthroplasty offers numerous benefits, potential complications include:
- Implant Loosening: Proper surgical technique and patient selection are vital to minimize this risk.
- Fractures: Intraoperative fractures can occur, particularly in patients with compromised bone quality.
- Infection: Strict aseptic techniques and perioperative antibiotics are employed to reduce infection rates.
11. Long-Term Outcomes and Success Rates
Studies have shown promising results with short-stem implants, with high survival rates and satisfactory functional outcomes. However, long-term data is still being collected, and ongoing research is essential to fully understand the durability and performance of these implants over time.
12. Comparing Short-Stem with Traditional Hip Replacements
When comparing short-stem to traditional hip replacements, key considerations include:
- Bone Preservation: Short-stem implants offer superior bone conservation.
- Patient Demographics: Younger, active patients may benefit more from short-stem designs.
- Revision Surgery: Bone preservation with short-stem implants can facilitate easier revision procedures if needed.
13. Patient Selection Criteria (continued)
- Younger Patients: Typically under 60 years old, who are more likely to require revision surgery later in life, benefit from the bone-preserving nature of short-stem implants.
- Active Individuals: People who lead an active lifestyle may experience improved biomechanics and faster recovery due to the more natural load distribution of short-stem implants.
- Good Bone Quality: Patients with healthy, dense bone in the proximal femur are ideal candidates, as this ensures optimal stability and reduces the risk of implant loosening or subsidence.
- Patients Seeking Faster Recovery: Short-stem implants, often placed using less invasive techniques, are associated with quicker recovery times, making them appealing to those who prioritize an expedited return to daily activities.
However, short-stem implants may not be suitable for patients with severe osteoporosis, complex deformities, or significant bone loss. In such cases, traditional long-stem implants may provide more reliable fixation.
14. Innovations and Future Directions in Hip Arthroplasty
Short-stem total hip arthroplasty represents a leap forward in joint replacement technology — but innovations are continuously evolving to improve outcomes further.
- 3D Printing and Patient-Specific Implants: Advances in 3D printing are enabling the creation of custom-designed short-stem implants tailored to each patient's unique anatomy. This personalization may improve stability, reduce wear, and enhance longevity.
- Biocompatible Coatings: New surface coatings, such as hydroxyapatite or porous titanium, promote better bone integration and enhance the longevity of the implant.
- Smart Implants: Emerging technologies may incorporate sensors within the implant to monitor load distribution, alignment, and early signs of loosening or wear, allowing for proactive management of complications.
- Minimally Invasive Robotic-Assisted Surgery: The use of robotic systems is becoming more prevalent in orthopedic surgery. These systems enhance precision in implant positioning, which is particularly beneficial for short-stem procedures where exact placement is crucial for stability.
- Tissue-Sparing Techniques: Future surgical approaches may further minimize soft tissue disruption, accelerating recovery while maintaining long-term stability and function.
15. Conclusion
Short-stem total hip arthroplasty is redefining the landscape of hip replacement surgery. By prioritizing bone preservation, improving biomechanics, and supporting faster recovery times, this innovative approach is particularly suited for younger, active patients and those seeking a more natural joint feel.
While long-term studies are ongoing, current data suggests that short-stem implants offer comparable — if not superior — outcomes to traditional long-stem designs. However, patient selection remains critical to ensure optimal results.
With advancements in implant materials, surgical techniques, and emerging technologies like 3D printing and robotic assistance, the future of short-stem total hip arthroplasty looks brighter than ever. For patients considering hip replacement, consulting with an experienced orthopedic surgeon who specializes in this technique is essential to determine whether a short-stem implant is the right choice for their individual needs.
Whether you're an active adult seeking faster recovery or a younger patient prioritizing bone preservation for future revisions, short-stem total hip arthroplasty offers a promising path to restored mobility, pain relief, and a better quality of life.
Comparison of Leading Short-Stem Implants
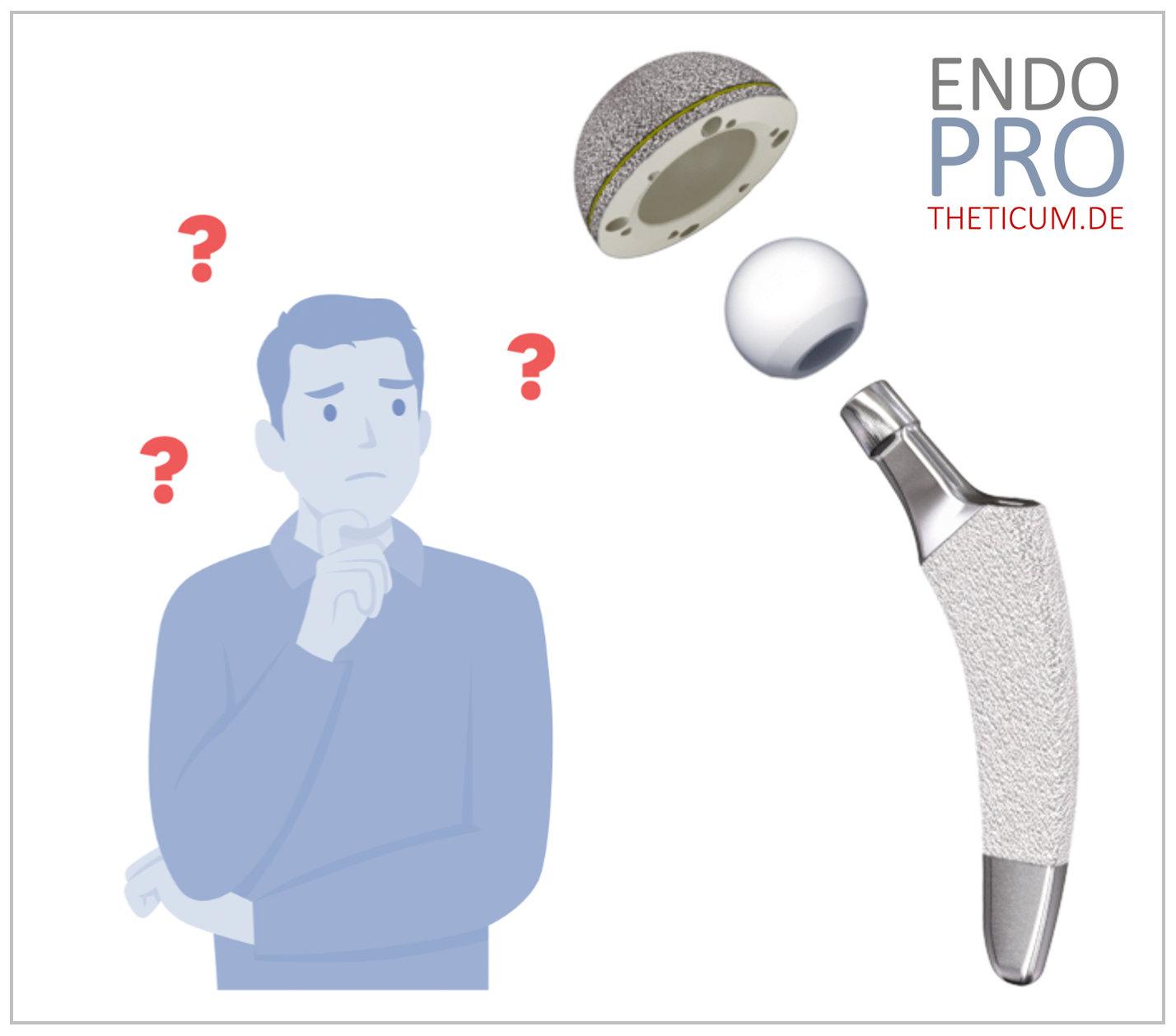
Short-stem implants are not one-size-fits-all. Below is an in-depth comparison of the most widely used and clinically studied models:
16.1. Optimys (Mathys)
- Design Features:
- Anatomically adapted stem with a lateral curvature that mimics natural femoral anatomy.
- Collarless design to allow for metaphyseal anchoring and physiological load transfer.
- Material: Titanium alloy with a roughened surface to promote bone integration.
- Advantages:
- Bone-preserving proximal fixation reduces the risk of thigh pain.
- Excellent rotational stability due to an optimized design that fits snugly in the metaphysis.
- Lower risk of stress shielding thanks to the anatomical load distribution.
- Clinical Outcome: Studies report high primary stability and low rates of migration. It’s the most succesful short-stem in terms of revision rates.
- Ideal Candidate: Young, active adults with good bone quality.
16.2. MiniHip (Corin)
- Design Features:
- Designed to preserve more of the femoral neck than other short-stem options, promoting natural biomechanics.
- Short, straight design that allows for easier insertion through minimally invasive approaches.
- Material: Titanium alloy with a hydroxyapatite coating to enhance osseointegration.
- Advantages:
- Enhanced stability due to greater femoral neck preservation.
- Allows for improved leg length and offset restoration, leading to more natural hip mechanics.
- Excellent results in patients with slightly abnormal proximal femur anatomy.
- Clinical Outcome: Long-term studies show promising survivorship, with bone remodeling patterns similar to natural hip biomechanics.
- Ideal Candidate: Patients with abnormal femur anatomy or those who prioritize natural hip function and joint mechanics.
16.3. Metha (Aesculap)
- Design Features:
- Tapered stem for enhanced metaphyseal fixation.
- Material: Titanium alloy with a roughened surface for long-term fixation.
- Advantages:
- Excellent primary stability with early weight-bearing encouraged.
- Allows for individual anatomical reconstruction, ideal for complex hip shapes.
- Clinical Outcome: Reported to show excellent survivorship with low rates of loosening, even in challenging anatomical scenarios.
- Ideal Candidate: Patients with excellent bone quality to ensure metaphyseal fixation.
16.4. Nanos (Smith & Nephew)
- Design Features:
- Short, curved stem with metaphyseal fixation and reduced distal stress.
- Collarless design for enhanced proximal load transfer.
- Material: Titanium alloy with a porous surface for enhanced bone bonding.
- Advantages:
- Preserves maximum bone stock, making it ideal for future revisions.
- High primary stability, even with less invasive surgical techniques.
- Low incidence of thigh pain, common in longer stems.
- Clinical Outcome: Proven long-term durability and excellent rotational stability, even in younger and active patients.
- Ideal Candidate: Younger patients who may require future revisions or those seeking faster recovery with less invasive techniques.
16.5. Fitmore (Zimmer Biomet)
- Design Features:
- Unique modular stem geometry designed to optimize proximal fill for stability.
- A progressive curvature adapts to different femoral morphologies.
- Material: Titanium alloy with a porous coating for faster bone in-growth.
- Advantages:
- Versatile design suitable for various femoral shapes and sizes.
- Supports minimally invasive surgical techniques.
- Maintains natural femoral loading to prevent stress shielding.
- Clinical Outcome: Demonstrated excellent clinical outcomes with low rates of loosening and subsidence.
- Ideal Candidate: Patients with varying femoral anatomies, particularly those needing customization for leg length or offset.
Final Thoughts on Choosing a Short-Stem Implant
Each short-stem implant design offers unique benefits suited to different patient profiles.
- For young, active patients prioritizing bone preservation and future revision options, Nanos and MiniHip stand out.
- For patients with anatomical abnormalities, Metha and Fitmore provide more customization and adaptability.
- For straightforward primary hip replacements with a focus on early weight-bearing and faster recovery, Optimys delivers robust stability and load distribution.
In the end, the best short-stem implant depends on a combination of patient anatomy, surgeon experience, and long-term treatment goals.
Patient Decision Guide: Choosing the Right Short-Stem Implant
When patients hear they need a hip replacement, the variety of implant choices can feel overwhelming. This section breaks it down step by step, helping patients and caregivers make informed decisions alongside their surgeon.
19.1. Step 1: Understand Your Personal Needs
Before diving into implant brands, it's important to evaluate what you need from your hip replacement. Ask yourself:
- How active do I want to be after surgery?
- If you enjoy sports, hiking, or dancing, implants designed for high stability (e.g., Nanos, MiniHip) may suit you best.
- How important is bone preservation for me?
- Younger patients who may need a revision in the future should consider bone-preserving designs like Nanos or MiniHip.
- Do I have any unique anatomical considerations?
- Patients with anatomical variations may benefit from adjustable modular implants like Metha or Fitmore.
19.2. Step 2: Discuss with Your Surgeon
Bring your questions to the consultation. Here’s what to ask:
- Which short-stem implants do you use most often, and why?
- What are the pros and cons of each implant for my specific case?
- How does my bone quality and hip anatomy affect the choice?
- What are the long-term results for this implant in patients like me?
19.3. Step 3: Consider Your Long-Term Goals
A hip replacement is designed to last 15–25 years or more. Think about:
- Future revision surgery: Short-stem implants help preserve bone, which can make future revision easier.
- Return to activity: If you want to return to strength training, cycling, or other low-impact sports, ensure your implant supports those goals.
- Lifestyle factors: For example, frequent travelers might prefer an implant with faster recovery potential.
Post-Surgery Rehab Guide: Getting Back on Your Feet After Short-stem THA
The journey doesn’t end after surgery — rehab is where the real transformation happens. A successful recovery helps ensure the implant stays stable, functional, and pain-free for years to come.
20.1. Phase 1: Early Recovery (0–6 Weeks)
Goal: Protect the implant and rebuild basic mobility.
- Weight-bearing: Most short-stem implants allow immediate weight-bearing, but follow your surgeon’s guidance.
- Exercises: Gentle ankle pumps, leg slides, and seated knee extensions prevent stiffness and blood clots.
- Walking: Start with a walker or crutches, then gradually transition to a cane as your strength improves.
✅ Pro tip: Avoid deep bending, twisting, or crossing your legs to prevent dislocation during the first 2 weeks.
20.2. Phase 2: Strength and Mobility (6–12 Weeks)
Goal: Improve hip stability and flexibility.
- Exercises: Include seated leg raises, light squats, and side leg lifts to build hip strength.
- Balance training: Standing on one leg (with support) improves stability.
- Walking progression: Increase daily walking distances, aiming for 20–30 minutes per day.
✅ Pro tip: Swimming and stationary cycling are excellent low-impact options to maintain cardio fitness.
20.3. Phase 3: Return to Activity (3–6 Months)
Goal: Regain full function and return to light activities.
- Strength training: Focus on compound movements like squats and lunges — but avoid heavy weights to reduce implant stress.
- Cardio: Walking, swimming, and cycling remain ideal. Avoid running or jumping sports to prevent implant wear.
- Stretching: Incorporate gentle stretches for the hip flexors, glutes, and hamstrings to prevent stiffness.
✅ Pro tip: Listen to your body. Mild soreness is normal, but sharp pain isn’t — consult your surgeon if needed.
20.4. Long-Term Maintenance (6 Months and Beyond)
Goal: Maintain strength, prevent complications, and enjoy your new hip!
- Strength: Continue light weight training, focusing on controlled movements and proper form.
- Cardio: Low-impact exercises like walking, swimming, and cycling remain the best long-term choices.
- Lifestyle modifications: Keep a healthy weight to reduce unnecessary stress on the implant.
✅ Pro tip: Regular follow-ups are essential. X-rays monitor implant stability and check for loosening or wear.
Addressing Common Concerns: FAQs from Patients regarding short-stem implants
To wrap things up, let’s tackle a few common questions:
Q: Can I still play sports with a short-stem implant?
A: Yes — but low-impact activities like swimming, cycling, and strength training are safest. High-impact sports like running or tennis may accelerate implant wear.
Q: How long do short-stem implants last?
A: Studies show excellent durability, often matching or exceeding traditional longer stems. Many short-stem implants demonstrate
95%+ survivorship at 10–15 years.
Q: Is a short-stem implant better for younger patients?
A: Typically, yes! Short-stem implants preserve more bone, making future revisions easier — an important consideration for younger, active patients.
Q: Are there any downsides to short-stem implants?
A: While the benefits are impressive, short-stem implants may not be ideal for patients with severe osteoporosis or very unusual hip anatomy. Your surgeon will help decide what’s best for you.
Final Thoughts: A New Era for Hip Replacement
Short-stem total hip arthroplasty represents a revolution in hip replacement surgery. From faster recovery to improved biomechanics and bone preservation, short-stem implants are transforming patient outcomes — particularly for younger, active adults.
By understanding the different designs, weighing the pros and cons, and following a dedicated rehab program, patients can feel confident they’re making the best decision for their health and future mobility.
Take the Next Step: Is Short-Stem Total Hip Arthroplasty Right for You?
Hip pain shouldn’t control your life — and with modern advancements like short-stem total hip arthroplasty, it doesn’t have to. These innovative implants offer faster recovery, better bone preservation, and a more natural feel compared to traditional long-stem designs.
Whether you’re an active adult eager to maintain mobility, a younger patient looking to preserve bone for future revisions, or someone seeking a smoother, faster recovery — short-stem technology could be the perfect fit for your needs.
👉 Your next step?
- Talk to your orthopedic surgeon about short-stem implants and whether they’re a good option for your unique situation.
- Ask specific questions about implant brands, surgical techniques, and expected outcomes.
- Explore second opinions if you’re unsure — especially if your lifestyle or age makes bone preservation important.
The future of hip replacement is here — and it’s lighter, stronger, and more patient-focused than ever before. Take control of your hip health today — because you deserve a pain-free, active future.
TERMIN VEREINBAREN?
Gerne können Sie einen Termin sowohl telefonisch, als auch online vereinbaren.